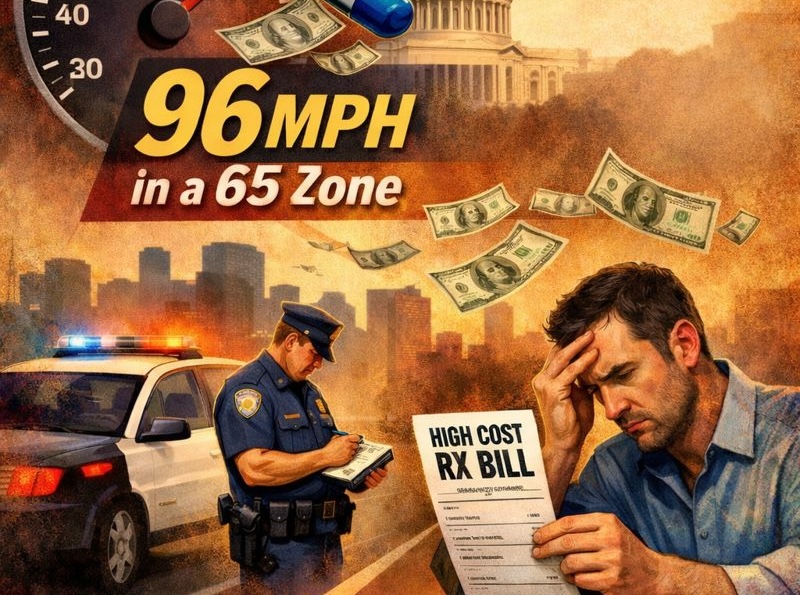
Drugmakers Are Speeding, and Patients Are Paying the Ticket
By ALDP Co-Founders Michael Glassner and Jason Young
January 28, 2026
Just before Christmas, news outlets across the country reported that more drugmakers had reached agreements with the White House to lower prices. The message was unmistakable: President Trump’s pressure was working, restraint was taking hold, and the industry was finally moving in the right direction.
Then the calendar flipped.
For 2026, pharmaceutical manufacturers have planned routine list-price increases on hundreds of branded medicines, with a typical hike of about 4 percent – well above current inflation, which is running closer to 2.7 percent. This news didn’t grab as many headlines.
President Trump did not merely endorse lower drug prices in the abstract. He publicly demanded action, convened manufacturers, and stood in the Oval Office as deals were announced. Now the industry has reverted to business as usual, increasing prices that are already the highest in the world. This is not restraint. It’s a calculated bet that they can outlast political pressure. Or that a few deals insulate them from wider accountability.
Drugmakers insist these increases are “modest.” They are not.
A 4 percent drug price hike in a 2.7 percent inflation environment is nearly 50 percent too high. It’s the equivalent of driving 96 miles an hour in a 65 zone and hoping no one notices. In a market measured in the hundreds of billions of dollars, that excess speed translates into billions more extracted from patients and taxpayers every year.
Prescription drugs are not a marginal expense. It’s either impractical or impossible for patients to comparison-shop for chemotherapy or insulin. Employers cannot easily absorb repeated price hikes without passing costs along. And public programs cannot walk away. Medicaid prescription drug spending has been growing at double-digit rates on average in recent years – far faster than inflation and faster than most state revenues.
List-price increases ripple through the system. They drive patient cost-sharing, inflate cash-pay prices, and raise baseline spending for state and federal programs. Those higher baselines then become the starting point for the next round of increases. The ratchet only turns one way.
The industry argues that these increases are necessary to support innovation. But innovation is not priced in a vacuum. If prices truly reflected costs, Americans would not routinely pay two to three times what patients in other developed countries pay for the same medicines made by the same companies. Nor would prices continue to rise year after year on drugs that have long since recouped their research and development costs. Other countries get innovation and lower prices, while Americans are told we have to pick one.
This is not just a federal issue. State legislatures are reconvening right now, and they face a clear choice.
They can bring real fiscal discipline to prescription drug spending, using the tools available to them to protect state budgets and patients. Or they can succumb to inertia – a pattern in which industry lobbyists deny there’s a problem, deflect blame to other parts of the health system, and delay reform. With drug spending steadily crowding out other public priorities, it’s time to act.
States have tools available, including Prescription Drug Affordability Boards – independent boards designed to review excessive price increases. Several states have already enacted them. More should follow in 2026, before July brings the next round of price hikes.
State lawmakers’ choice also comes with political clarity. 2026 is an election year. Voters may not follow Consumer Price Index reports, but they understand when prices keep rising faster than the economy and when state budgets feel perpetually squeezed. Standing with voters against unjustified drug price increases is not a gamble. It is common sense.
Drugmakers point to selective price cuts on a handful of medicines as evidence of progress. But isolated reductions do not offset a system that still relies on routine, above-inflation increases across hundreds of products. Incremental restraint does not excuse structural excess.
Inflation has cooled considerably, and the President has drawn a line on drug prices. If states act now, patients, small businesses, taxpayers, and state budgets all benefit. But only if industry faces real consequences – not just presidential pressure, but state-level processes and accountability on what manufacturers can charge. Industry can’t just keep speeding, betting that no one will pull them over.