State Round-up Part 2: States on A Concerning Path – Risking Rural Pharmacy Access, Ignoring Drug Prices
By ALDP Co-Founders Michael Glassner and Jason Young
In Part 1 of our state round-up, we highlighted states making progress on prescription drug affordability through Prescription Drug Affordability Boards and insulin price caps – policies that address the root cause of unaffordable medications by checking manufacturers’ unchecked pricing power.
In Part 2, we need to talk about states moving in the wrong direction. Legislation pending in Tennessee, Oklahoma, and Arizona could hurt the populations ALDP advocates for: veterans, seniors, people living in rural communities, people with disabilities, and those who are uninsured or underinsured – by both increasing costs and limiting access and choice.
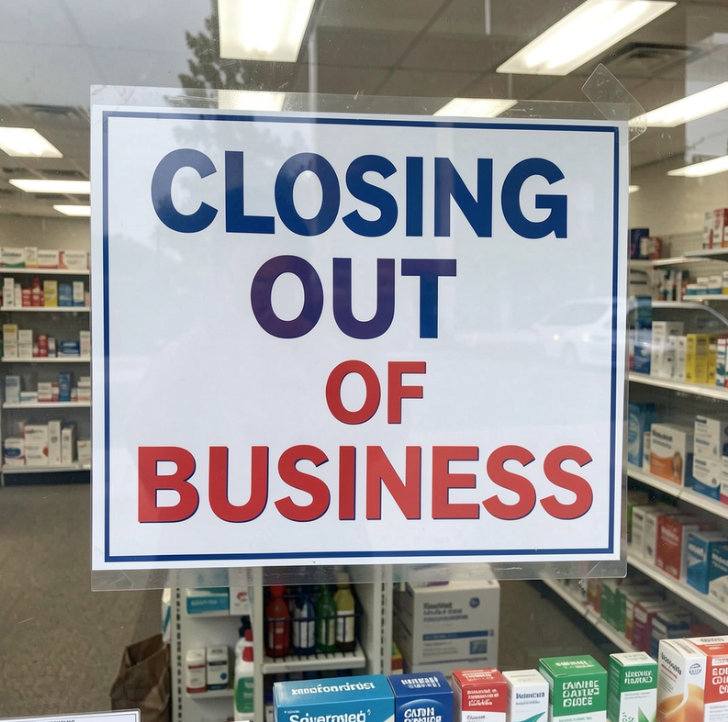
The pending legislation would restrict pharmacy ownership based on corporate structure – determining which businesses can and cannot operate pharmacies in their states. The stated goal is protecting rural pharmacy access. The actual result would be the opposite: fewer pharmacies and pharmacy services for communities that can least afford to lose them. When a rural pharmacy closes, it’s not just an inconvenience – it’s a health care crisis for communities that lack options.
Every Rural Pharmacy Is An Asset
The bills in Tennessee (SB 2040 / HB 1959), Oklahoma (HB 4457), and Arizona (SB 1545) target some pharmacies, but not others, based on ownership structure and would force affected pharmacies to find a buyer or close. The legislation requires the sale by a specific date, often within a year or two, or the pharmacy will lose its license. That’s disruptive in three ways: it forces a fire sale, it closes pharmacies, and it leaves rural residents without options or access.
We believe rural communities need every type of pharmacy serving patients today – independent retail, chain retail, mail-order, and specialty pharmacies. Creating a level playing field for all pharmacies is fundamentally different from legislation that mandates sell-offs and closures – closing down entire categories of pharmacies. This legislation doesn’t solve the affordability problem; it creates access problems while leaving manufacturer pricing power untouched. It could also reduce competition, while adding transportation and time costs.
Mail-Order Pharmacy Serves Critical Populations
In our advocacy work, we’ve learned about the patterns of pharmacy use that underscore the need to preserve all access channels:
- The greatest number of people use chain retail pharmacies
- Another strong contingent primarily uses independent pharmacies, and
- A small but important group – often seniors, veterans, and those with mobility issues – relies primarily on mail-order pharmacy services.
Ensuring medications and pharmacy services reach rural areas requires a both/and approach – not forced choices between pharmacy types.
Consider the personal stories we’ve heard. Military families tell us they depend on mail-order pharmacy given frequent deployments and moves, Data shows TRICARE families may use mail-order at rates four times higher than the general public. Rural communities depend on both independent and chain retail locations. Importantly, seniors depend on convenient access regardless of ownership structure; data tell us seniors are some 50% more likely to rely on mail-order pharmacy services. Policies that mandate closures of functioning pharmacies hurt patients.
Put simply: legislation mandating pharmacy closures and eliminating mail-order options could significantly disrupt access, particularly in rural areas.
Path Forward: Address Manufacturer Pricing, Preserve Pharmacy Access
When Americans are asked about pharmacy policy, they typically say they want bold action on the real problem – excessive manufacturer pricing – without eliminating the pharmacies and services they depend on.
What actually threatens rural patients? The same thing threatening health care affordability everywhere: unsustainable drug prices.
Consider the blood-thinner Eliquis. A 30-day supply costs $346 in the United States, but in Canada, it’s $100 to $150 for the brand name, and less still for generic apixaban, which is available there but has been blocked from the U.S. market. Closing your pharmacy does nothing to lower that $346 price tag. It just adds transportation and time costs when you travel farther to fill your prescription.
If states want to protect rural pharmacy access, here’s what would work:
Address drug affordability directly. When states establish Prescription Drug Affordability Boards and set upper payment limits, they create more predictable economics for everyone– including rural patients and pharmacies.
Support rural pharmacy operations. Some states have created grant programs, loan forgiveness for pharmacists in underserved areas, or technical assistance for independent pharmacies. These directly address rural face pharmacy challenges without restricting which business models can serve communities.
Don’t restrict business models that are working. If a pharmacy is operating today, why would state legislators make that illegal? The goal should be more options for rural communities, not fewer.
Whose Interests Are Really Being Served?
It’s worth asking who benefits from legislation that restricts pharmacy ownership. Not rural communities – they lose many pharmacies in operation and serving them today. Not patients – they lose access to care. The legislation under consideration goes further than “leveling the playing field” – it significantly tilts the field in favor of one pharmacy business model over another.
We believe policymakers should be skeptical of any proposal that reduces competition in health care markets while claiming to help patients.
Every Type of Pharmacy Matters
Our country needs every type of pharmacy serving patients today – independent retail, chain retail, specialty, and mail-order pharmacies. Each serves different patient needs and community circumstances. Removing some of those players from the field is not helpful to meeting patients’ needs. Closing down entire categories of pharmacies doesn’t solve the affordability problem; it only creates new access problems while leaving manufacturer pricing power untouched.
Rural communities deserve better than legislation that restricts their options while ignoring the actual drivers of pharmacy closures.
Legislative sessions are short. States have limited time and attention to dedicate to health care policy. Spending that time on legislation that will close rural pharmacies instead of saving them is a tragic waste – and rural patients will pay the price.
That’s not the laboratory of democracy working. That’s special interests winning while patients lose.